New trial shows mucus-thinning drugs are ineffective in people with bronchiectasis
A major clinical trial funded by the National Institute for Health and Care Research (NIHR) led by Queen’s has shown mucus-thinning drugs have little effect on acute flare-ups of respiratory symptoms in people with non-cystic fibrosis bronchiectasis.
The results were presented at the European Respiratory Society (ERS) Congress 2025 conference in Amsterdam and have been published in the New England Journal of Medicine.
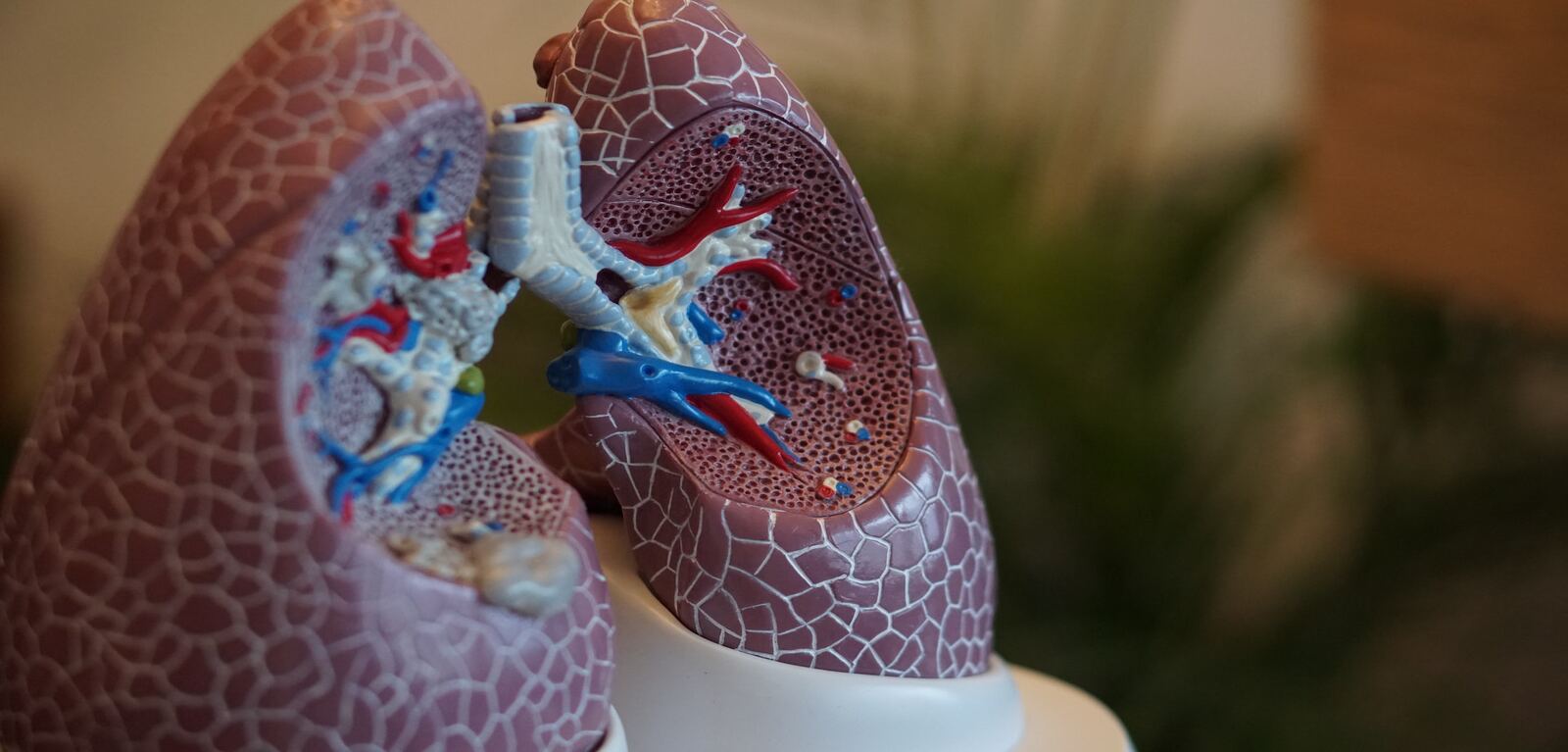
Non-cystic fibrosis bronchiectasis is a chronic lung condition where airways become permanently widened due to recurrent infections and inflammation.
Due to these widened airways, phlegm (sputum) can build up, increasing the risk of getting infections, as the built-up phlegm makes it easier for bacteria to get trapped in the airways.
Mucus-thinning drugs, or mucolytics and expectorants, are used to manage this mucus and help prevent recurrent infections in patients with bronchiectasis.
Professor Judy Bradley, Lead Physiotherapy Investigator from the Wellcome-Wolfson Institute for Experimental Medicine at Queen’s University Belfast explains: “Bronchiectasis guidelines are inconsistent in terms of evidence for the effectiveness of mucoactive agents, and their use varies geographically. Large trials are needed to assess their safety and effectiveness to ensure people with bronchiectasis are being given the best treatment and care.”
The CLEAR trial looked at 288 adults with non-cystic fibrosis bronchiectasis across the UK for over 52 weeks. The researchers determined the clinical and cost -effectiveness of hypertonic saline HTS (6%) and carbocisteine, the two most used mucoactive agents, for airway clearance versus usual care in bronchiectasis.
The team found that neither hypertonic saline nor carbocisteine significantly reduce pulmonary exacerbations in patients over the 52 weeks.
Professor Judy Bradley, trial lead and Director of Clinical Research Facility at Queen’s University Belfast continues: “Our findings show there is no benefit in prescribing hypertonic saline or carbocisteine to prevent exacerbations in people with bronchiectasis. This provides clarity for patients, clinicians and policymakers and should inform future guideline updates.”
The trial was funded by the National Institute for Health and Care Research (NIHR) Health Technology Assessment (HTA) Programme.
Media
Media inquiries to Sian Devlin at s.devlin@qub.ac.uk