Queen’s University Belfast leading £1.2m project to revolutionise medical treatment
Queen’s University Belfast are leading a £1.2m project to improve drug delivery for a range of illnesses.
The grant, awarded by the Engineering and Physical Sciences Research Council (EPSRC), part of the UK Research and Innovation, will accelerate the development of microarray patches to make them available to patients worldwide.
Microarray patches offer practical solutions to many of the barriers faced with drugs delivered orally or by injection, depending on their makeup. Although there has been significant scientific progress in microarray technology, a medicinal product is yet to be commercialised, a challenge which this collaborative project aims to address.
Traditional pharmaceutical medicines contain small molecules that treat the symptoms of a disease. Treatments with small molecules delivered over longer periods of time are often administered by injection to enable slow-release treatment for example, injections for TB and HIV.
Biopharmaceuticals are larger molecules (e.g., proteins), which target the underlying mechanisms and pathways of a disease that are not accessible with traditional medicines. When taken orally, larger molecules drugs are typically broken down in the stomach. This creates a challenge with ensuring it reaches the target site, meaning biopharmaceutical drug delivery is often achieved via injection.
Microarray patches enable drug treatments with both small or large molecules to be delivered efficiently, eliminating the need for injections. Replacing an injection with a microarray patch could have huge implications for the advancement of medical care.
Most injections are still administered in a healthcare setting. However, healthcare worldwide continues to be under pressure due to the COVID-19 pandemic. At-home administration of injected medicines would reduce workload, freeing up healthcare workers to focus on diagnosis and treatment of diseases other than COVID-19. Complexities of storage, distribution and administration, needle phobia and the difficulty of domestic disposal of potentially-contaminated sharps have highlighted the urgency with which alternative delivery models for injectable drugs and biopharmaceuticals must be found.
Microarray patches are a discreet, easy-to-use technology and painlessly penetrate the top layer of skin to deliver a drug. The patch surface that contacts the skin comprises many tiny projections that pierce the stratum corneum without causing any pain. These micro-projections create new pathways across the stratum corneum and can be designed to either enable rapid or controlled and continuous drug delivery. Consequently, microarray technology has the potential to revolutionise the administration of both biopharmaceuticals and long-acting small molecules that are otherwise unable to be delivered across the skin.
Project leader Professor Ryan Donnelly from Queen’s School of Pharmacy said: “Our research to date has suggested that microarray patches will be an effective replacement for conventional needles for a number of indications, whether it’s slow-release delivery for HIV treatment or pain-free vaccination. If we can replace the need for a range of drugs and vaccines to be given by needle-and-syringe injection with a minimally-invasive and painless patch, healthcare organisations, such as the NHS, could soon benefit from reduced costs due to shorter hospital stays and more reliable drug dosing, resulting in enhanced patient quality-of-life.
“Specific anticipated benefits include improved disease control, faster detection of disease, avoidance of under- or over-dosing, and better adherence to treatment. The pain-free administration of medicines by microarray patches offers particular advantages for patients at the extremes of the age spectrum enabling more frequent monitoring and multiple drug dosing to be achieved in a convenient manner. Importantly, in the present circumstances, at-home treatment/diagnosis and keeping people away from healthcare settings will help to reduce the spread of COVID-19 to vulnerable in-patients and healthcare workers.”
The three-year collaborative project will bring together experts from academia, pharmacy and clinical settings. The team includes Queen’s University Belfast, Loughborough University and The University of Bath in conjunction with clinicians, leading companies in pharmaceutical materials and manufacture, and advanced microscopy, and the National Physical Laboratory.
Dr Begona Delgado-Charro, from the University of Bath, added: “We’re delighted to be contributing to this important, translational research project, which will bring a cutting-edge technology to a range of clinical applications. Our role in the work addresses two specific issues. First, we’ll be assessing the fate of the polymers that the microneedles are made from once they are inserted into the skin. Second, we’ll be proactively engaging with regulators, doctors and industry to move things forward in bringing to market drug products that take advantage of this exciting approach.”
Professor Donnelly concluded: “We are delighted with this level of support from EPSRC, which will allow us to answer key questions to facilitate translation of microarray technology to the market for the benefit of patients worldwide. One team could not tackle such a multi-faceted task alone and so we have brought together a consortium of world-leading experts to accelerate microarray patch development.”
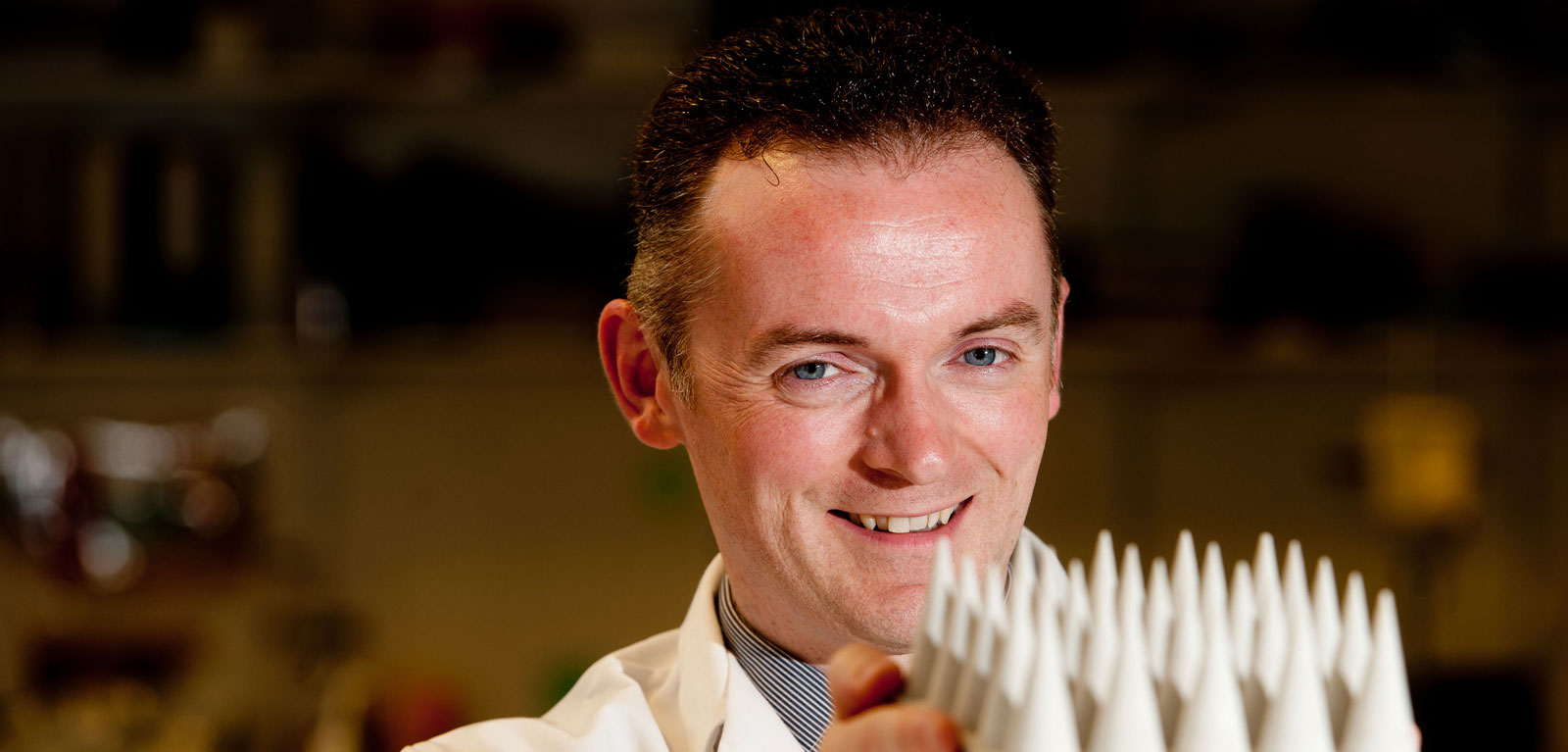
Featured Expert
Media
Media enquiries to comms.officer@qub.ac.uk