New study finds combined wastewater and individual testing best for COVID-19 detection
A new large-scale study led by researchers from Queen’s University has shown that combined wastewater testing and testing of individuals is the most effective way to track SARS-CoV-2, the virus that causes COVID-19.
Together, these tests offer a faster and more comprehensive public health response not only for SARS-CoV-2 and COVID-19, but also for other viruses like the flu, norovirus, or emerging threats we don’t yet know about.
The results have been published in Water Research.
The study involved researchers from across Queen’s including the Wellcome-Wolfson Institute for Experimental Medicine (WWIEM), the Institute for Global Food Security (IGFS)/School of Biological Sciences (SBS), the School of Natural and Built Environment (Geography) and the School of Pharmacy (SoP).
It also included key contributions from partner organisations; the Regional Virus Laboratory of the Belfast Health and Social Care Trust (BHSCT), the Northern Ireland Department of Health Public Health Agency (PHA), and Northern Ireland Water (NI Water), who facilitated access to wastewater treatment plants across the region.
The research was supervised by Professor David A. Simpson, Professor of Genomics from the WWIEM, with wastewater sequencing led by Professor of Environmental Microbiology, John W. McGrath and virological insight provided by co-corresponding author, Dr Connor G. G. Bamford from the IGFS/SBS.
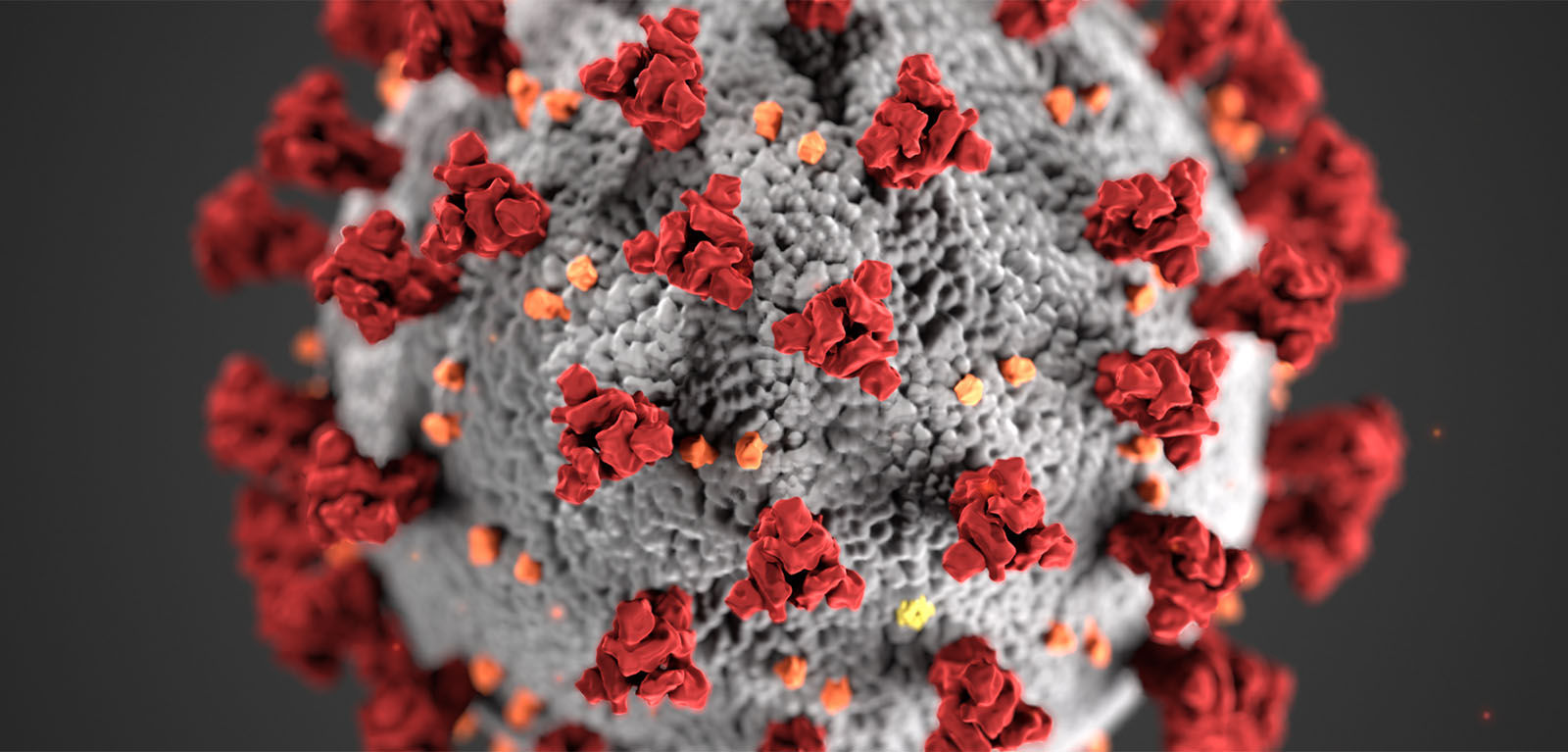
Lead Author on the study, Dr Evan P. Troendle, a Postdoctoral Researcher from the Wellcome-Wolfson Institute for Experimental Medicine at Queen’s University Belfast explains: “When someone is infected with a virus like SARS-CoV-2, traces of it are shed in their bodily waste and end up in the sewage system.
“That wastewater can then be tested to detect and track viruses at a community level. This technique offers a powerful, anonymous, and cost-effective way to monitor infections across entire populations.”
To conduct their study, the team analysed the genetic material in more than 4,000 wastewater samples between late 2021 and early 2023, representing over one million people across Northern Ireland, and compared these with more than 23,000 individual clinical samples.
Using whole genome sequencing, a technique that “reads” the virus's genetic code, genetic changes were then tracked and measured to see how they changed over time.
The results found that each method provides unique insights but combining them gives the clearest and most complete view of how viruses spread, how and where new variants emerge, and where and when public health interventions, such as surge testing, enhanced surveillance, or clinical resource allocation, may be needed.
Explaining the significance of the results, Dr Troendle continues: “This is the first study to sequence and compare wastewater and clinical samples in Northern Ireland at a large scale. Even as individual testing became limited, wastewater sequencing continued to reveal critical changes in the virus, including the appearance of new mutations, leading to different strains.
“This study provides a blueprint for future pandemic preparedness, where routine wastewater monitoring could augment existing surveillance for disease outbreaks, not only of SARS-CoV-2, but of other pathogens like influenza or norovirus. Crucially, this would ensure that public health systems are equipped to detect future, as-yet-unknown threats.”
The study was funded by the Belfast Health and Social Care Trust (BHSCT), the Northern Ireland Department of Health, the Public Health Agency (PHA), the Department of Agriculture, Environment and Rural Affairs (DAERA), and the COVID-19 Genomics UK (COG-UK) consortium.
Media
Media inquiries to Sian Devlin at s.devlin@qub.ac.uk